It starts with pain that doesn’t feel ordinary
Not all cramps are the same. Some feel sharper. Deeper. They don’t leave with rest. Or heat. Or pills. They stay. Sometimes during periods. Sometimes in between. The pain spreads to the back. Or legs. Or stomach. It’s hard to name where it begins.
That’s how endometriosis hides. Behind familiar discomfort. It doesn’t wave a flag. It blends in. Until it doesn’t. Until you start avoiding plans. Counting hours. Holding your breath in meetings. That’s when it becomes more than monthly pain.
The pain shows up even when there’s no bleeding
It’s not just a period problem. Pain can come while ovulating. Or after. Or during sex. Sometimes even while using the bathroom. There’s no clear pattern. It arrives quietly. Without permission. And it stays too long.
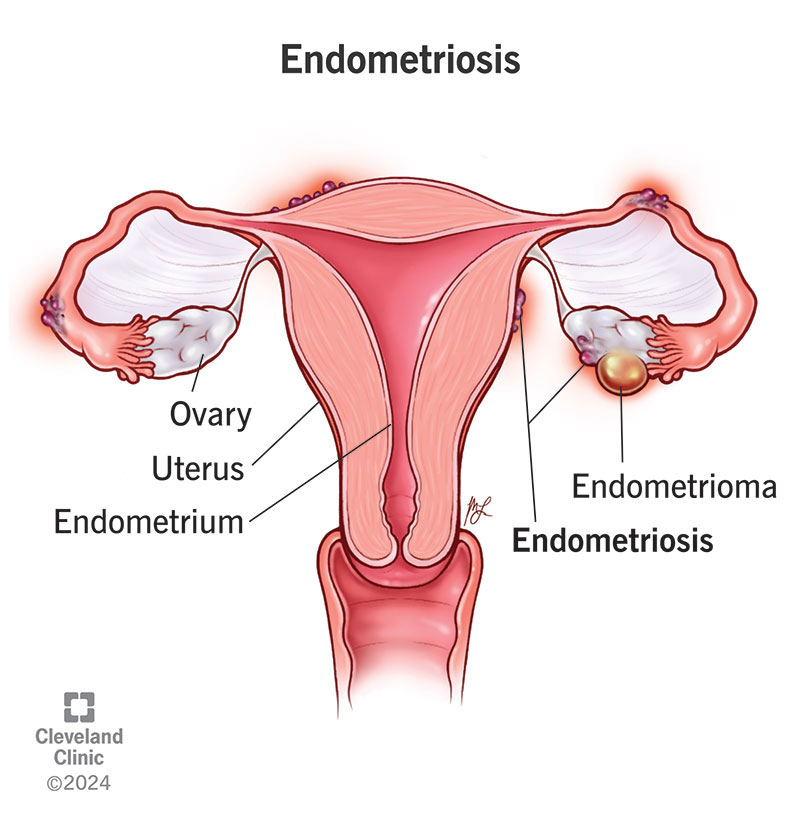
Endometrial tissue grows where it shouldn’t. On the ovaries. Behind the uterus. Along the pelvis. Each month, it responds to hormones like the uterus does. But it has nowhere to exit. So it swells. Breaks down. And causes inflammation.
Not every person with endometriosis feels the same
Some have heavy bleeding. Some don’t. Others have digestive issues. Bloating. Nausea. Diarrhea. Or constipation. Others feel extreme fatigue. Not tiredness—exhaustion that stops your day.
Fertility problems may appear later. Or not at all. That’s why diagnosis takes time. There’s no single symptom. Just a pattern that doesn’t quite match anything else. And many learn to ignore it.
Diagnosis isn’t always straightforward
Scans don’t always show it. Blood tests miss it. The pain is real, but the proof isn’t obvious. That’s why many people wait years for answers. It’s often misdiagnosed as IBS. Or pelvic infection. Or stress.
Sometimes doctors don’t believe the symptoms. Or they minimize them. The diagnosis usually comes through laparoscopy. A small surgery. A look inside. That’s when the truth becomes visible.
Treatment begins with managing the pain
There’s no cure. But there’s relief. The first step is usually medication. Anti-inflammatory drugs. Hormonal birth control. Pills. Patches. Rings. They reduce or stop menstruation. Less bleeding means less inflammation.
If pain continues, stronger treatments follow. Hormonal suppressants. GnRH agonists. Progestins. These lower estrogen. That slows the tissue’s growth. But side effects happen. And not everyone responds the same.
Surgery can help, but it doesn’t guarantee relief
Laparoscopic surgery removes visible endometrial tissue. It can ease pain. Improve fertility. But it’s not permanent. The tissue might return. Pain might come back. Sometimes quickly. Sometimes after years.
Hysterectomy is sometimes suggested. Especially when symptoms are severe. But even that doesn’t always fix everything. Because endometriosis isn’t just about the uterus. It’s about where that tissue spreads.
Lifestyle changes don’t cure it, but they help
Food matters. Some avoid gluten. Others reduce red meat. Anti-inflammatory diets may help some. Gentle movement eases the body. Yoga. Stretching. Walking. Not to fix—just to soften.
Stress adds layers. So finding ways to rest matters. Sleep. Warm baths. Silence. Support groups can ease the mental load. Not because the pain is imagined—but because being believed is healing too.
Emotional toll is part of the condition
Pain wears people down. Missing work. Canceling plans. Feeling misunderstood. It isolates. Makes you question your own body. Your own strength.
Depression and anxiety often walk beside it. Not because of weakness. But because chronic pain rewires your brain. That’s why treatment needs to address more than hormones. It needs space for grief, too.
It can affect fertility, but not always
Scar tissue might block the fallopian tubes. Or damage the ovaries. That affects conception. But many still get pregnant. Naturally. Or with help.
Fertility treatment options exist. IVF. Hormonal stimulation. Surgery before conception. Each path is personal. There’s no single outcome. Just options to explore.
Early diagnosis changes everything
Living with pain for years changes you. But catching it early prevents some of that. Knowing what it is helps you plan. Helps you speak. Helps you ask better questions.
Doctors are learning more. But awareness starts outside the clinic. It starts with people naming their pain. And others listening when they do.